Abstract
nts
Introduction
Myelodysplastic syndrome (MDS) is clinically and biologically heterogeneous. Although the pathobiology of MDS is complex and not fully understood, the development of MDS involves a series of genetic changes, which influence hematopoietic growth and differentiation, resulting in the accumulation of abnormal cells and the impairment of normal hematopoiesis. Recently, Lindsley et al. reported the difference in the mutation of MDS genes in adolescent and young adult (AYA) patients and elder patients. These results suggested that MDS in AYA patients was biologically different from MDS in elderly patients. In addition, AYA patients have some specific issues such as infertility, late complications, and psychological and social problems.
For AYA patients with MDS, similar to MDS patients of other age, allogeneic hematopoietic stem cell transplantation (HSCT) is the only curable treatment option. However, limited evidence was available indicating the effectiveness of allogeneic HSCT in the treatment of MDS in AYA patients, because about 90% of patients noted are usually in an older age group. Thus, we aimed to investigate the epidemiology of AYA patients with MDS who received allogeneic HSCT for the first time, and estimate prognostic factors after HSCT, using registry data of Japanese Data Center for Hematopoietic Cell Transplantation (JDCHCT).
Methods
We enrolled AYA patients aged 16-39 years from JDCHCT, who received allogeneic HSCT for the first time between January 2000 and December 2015. Active disease was defined as the presence of >5% blast in bone marrow and/or presence of blast in peripheral blood. We set the primary endpoint as the 5-year overall survival (5yOS).
Five-year cumulative incidence of relapse (5yCIR) and 5-year cumulative incidence of non-relapse mortality (5yCINRM) were also evaluated as secondary endpoints. OS was evaluated using the log-rank test. Other endpoints were evaluated using Gray's method. To evaluate the prognostic factor for 5yOS, we employed the multivariable Cox proportional hazards model. Covariates were as follows: age (16-29 vs 30-39), sex (male vs female), Performance Status (PS) according to the Eastern Cooperative Oncology Group (0-1 vs 2-4), disease status (active vs non-active), karyotype risk according to the International Prognostic Scoring System (IPSS, good vs intermediate vs poor), conditioning regimen (Reduced intensity conditioning regimen [RIC] vs myeloablative conditioning regimen), donor type (related bone marrow transplantation [BMT] or peripheral blood stem cell transplantation [PBSCT] vs unrelated BMT or PBSCT vs cord blood transplantation [CBT]), prophylaxis of graft-versus-host disease (tacrolimus-based vs cyclosporine A-based), and years of HSCT (2000-2007 vs 2008-2015).
Results
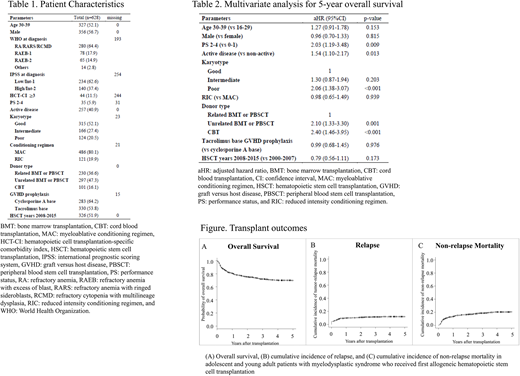
We analyzed 628 AYA patients with MDS who received HSCT for the first time. Patient characteristics are described in Table 1. Median age was 30 years, 327 patients (52.7%) were of age ≥30 years, and 356 patients (56.7%) were male. At diagnosis, 140 patients (37.4%) were at IPSS low or intermediate-1 risk. At HSCT, 257 (40.9%) patients had active disease and 315 (52.1%), 166 (27.4%), and 124 (20.5%) patients had good, intermediate, and poor risk karyotype, respectively. RIC was administered for 121 (19.9%) patients. Regarding donor type, 230 (36.6%) received related BMT or PBSCT, 297 (47.3%) received unrelated BMT or PBSCT, and 101 (16.1%) received CBT.
Regarding primary endpoint, 5yOS after allogeneic HSCT was 69.6% (65.6-73.2%) (Figure A). Five-year CIR and 5yCINRM were 11.9% (9.5-14.7%) and 20.7% (17.4-24.2%), respectively (Figure B, C). Regarding prognostic factors influencing 5yOS, active disease (adjusted hazard ratio [aHR]: 1.54, 95% confidence interval [95%CI]: 1.10-2.17, p-value = 0.013), poor karyotype (aHR: 2.06, 95%CI: 1.38-3.07, p-value < 0.001), PS 2-4 (aHR: 2.03, 95%CI: 1.19-3.48, p-value = 0.013), unrelated BMT or PBSCT (aHR: 2.10, 95%CI: 1.33-3.30, p-value = 0.001) and CBT (aHR: 2.40, 95%CI: 1.46-3.95, p-value < 0.001) were significantly associated with 5yOS, but other factors were not (Table 2).
Conclusion
In the present study, the epidemiology of AYA patients with MDS who received allogeneic HSCT for the first time, and the prognostic factors influencing 5yOS were evaluated. Our results provide physicians with additional information for the treatment of AYA patients with MDS.
Mori:Novartis Pharma: Research Funding; Astella Pharma: Honoraria; Shire Japan: Honoraria; Taisho Toyama Pharmaceutical Co: Honoraria; Japan Blood Products Organization: Honoraria; Eisai: Honoraria; Janssen: Honoraria; MSD: Research Funding; SHIONOGI: Honoraria; Pfizer: Honoraria; CHUGAI: Honoraria; Novartis Pharma: Honoraria; MSD: Honoraria; Ono: Honoraria; Celgene: Honoraria; Asahi Kasei: Research Funding; Kyowa Hakko Kirin: Honoraria. Tanaka:Bristol-Myers Squibb: Honoraria, Research Funding; Otsuka: Honoraria; Novartis Pharma: Honoraria; Pfizer: Honoraria. Ishiyama:Alexion Pharmaceuticals, Inc.: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.